Introduction
Intrauterine insemination (IUI) represents a significant milestone in assisted reproductive technology, offering hope to many couples struggling with fertility challenges. This relatively straightforward procedure has helped countless individuals achieve their dreams of parenthood, but success often depends on careful preparation and understanding of the process. Understanding how to optimize your chances of success with IUI is crucial for anyone considering this treatment or currently undergoing it. Despite in vitro fertilization and embryo transfer (IVF-ET) having a higher pregnancy rate, intrauterine insemination (IUI) remains a popular low-cost, less intrusive treatment for infertile couples. IUI clinical pregnancy rates (CPRs) varied from 10% to 20% every cycle, while substantial population-based data from the European Society of Human Reproduction and Embryology revealed a delivery rate of 9% per cycle. However, doctors continued to struggle with managing women over 35, particularly those who were 38 years old. To determine the best care for women over 35, this study analyzed IUI success rates by age, using multicenter data from four Chinese reproductive medical centers.
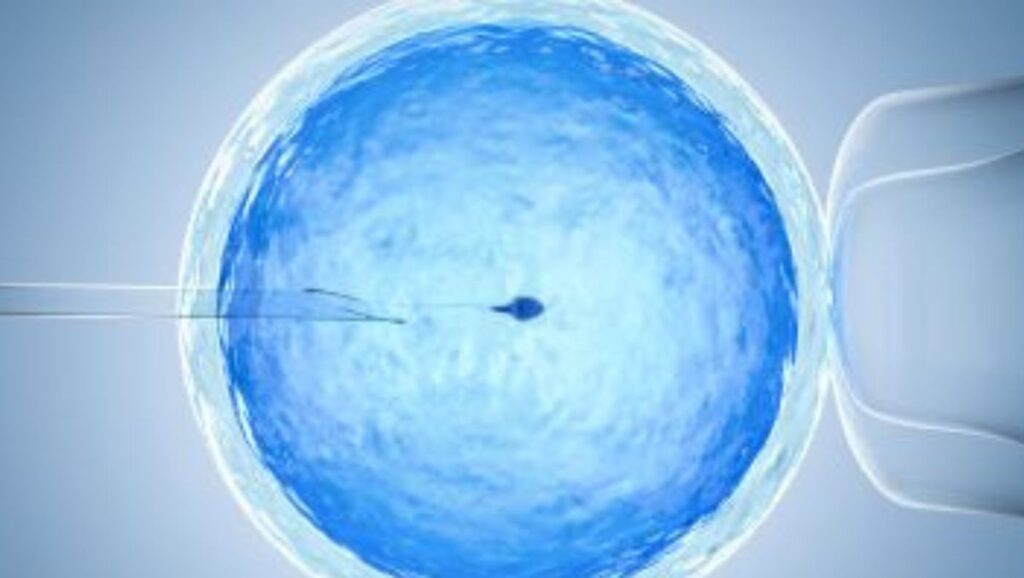
Understanding the basics of IUI
Intrauterine insemination involves the direct placement of specially prepared sperm into the uterus during the optimal time of a woman’s fertile window. This procedure bypasses potential cervical barriers and brings the sperm closer to the egg, increasing the likelihood of fertilization. IUI proves particularly beneficial for couples facing mild male factor infertility, cervical factor infertility, or unexplained infertility. Success rates typically range from 10% to 20% per cycle, varying significantly based on age, underlying fertility factors, and treatment protocol. Stimulated IUI does not help male infertility and has little influence on other conditions. Clomiphene citrate with IUI, the most prevalent IUI regimen, has 7% pregnancy rates every cycle. With pregnancy rates of 12% each cycle and multiple birth rates of 13%, FSH ovarian stimulation plus IUI therapy is just slightly better than observation. Mildly stimulated (1–2 follicles) cycles may lower expenses and multiple birth rates but need longer treatment cycles. IUI cycles may not need luteal phase assistance or premature luteinizing hormone spike prevention.
Preparing for IUI
Comprehensive preparation begins with thorough fertility testing for both partners. This includes evaluating ovarian reserve, checking fallopian tube patency, and conducting detailed semen analysis. Beyond medical evaluations, lifestyle modifications play a crucial role in optimizing fertility. A balanced diet rich in antioxidants, maintaining a healthy body mass index, and regular moderate exercise can significantly impact treatment outcomes. Stress management through techniques like meditation, yoga, or counselling helps create an optimal environment for conception. Many infertile couples worldwide choose IUI with or without OS as their initial therapy. When a couple goes through IUI or IUI/OS therapy, their medical care must include outcomes for the mother and baby, such as the problem of higher-order multiple pregnancies that are linked to IUI–OS. With a global focus on reducing maternal and perinatal mortality and morbidity, the World Health Organization’s (WHO) launched a multi-year project to review the evidence for normative guidance on IUI as a fertility treatment and its cost-effectiveness in low-resource settings.
Medical Preparations
The medical aspect of IUI preparation often involves careful hormonal stimulation when indicated. Doctors may prescribe fertility medications to boost ovulation or generate multiple mature follicles, thereby boosting the chances of conception. Regular monitoring through blood tests and ultrasounds helps track follicular development and determine the optimal timing for the procedure. We pay special attention to sperm preparation, employing techniques that choose the healthiest, most motile sperm for insemination. The luteal phase is crucial to a healthy pregnancy. The endometrium is dynamic, and the window of implantation occurs between days 19 and 24 of a spontanAssisted reproduction cycles (ART) use gonadotropin-releasing hormone analogues and an ovulation trigger to time final oocyte maturation, leading to substantial research on luteal phase abnormalities. ormalities. These medications inhibit pituitary luteinizing hormone release, which forms and activates the corpus luteum. Progesterone may increase pregnancy rates in ART cycles, but there is no consensus on the optimal formulation, route, initiation, and duration of treatment in fresh and frozen cycles. Hormonal dynamics and luteal phase differ in fresh and frozen-thawed cycles.
Maximising IUI Success During the Procedure
Timing is crucial for IUI success. Typically, we schedule the procedure 24-36 hours after detecting ovulation, either naturally or through trigger shots. Ultrasound monitoring helps verify follicle development and endometrial thickness, ensuring optimal conditions for implantation. The sperm washing process removes substances that could interfere with fertilisation while concentrating the healthiest sperm for insemination.
Post-IUI Care
We advise patients to maintain normal activities after the procedure, avoiding strenuous exercise or excessive stress. While bed rest isn’t necessary, taking it lightly for the remainder of the day can provide peace of mind. Understanding potential implantation signs helps manage expectations during the two-week waiting period. Common signs might include mild cramping or spotting, though their absence doesn’t indicate failure. Avoid stress-inducing workouts like weightlifting and running. IUI patients should not lift more than 4-5 kgs after treatment. IUI might induce cramps while lifting heavy goods.
Common Challenges and How to Overcome Them
Failed cycles can be emotionally devastating, but understanding that IUI often requires multiple attempts helps maintain perspective. Working with a fertility counselor or joining support groups can provide emotional support during difficult times. Each failed cycle offers valuable information that can help adjust future treatment protocols for better success. The study found that paternal age also predicts IUI success, decreasing after 35. Numerous research studies have examined paternal age and assisted reproductive outcomes with conflicting results. Men’s metabolic condition, including obesity and insulin resistance, affects fertility and neonatal health, according to recent studies. The risk of these illnesses grows with age; hence we think paternal age affects ART outcomes. Future research should include men’s BMI, insulin level, insulin resistance, and oxidative stress indicators.
Alternative Strategies to Boost IUI Success
Many patients explore complementary therapies alongside traditional treatment. Acupuncture may help improve blood flow to reproductive organs and reduce stress levels. Some clinics recommend combining IUI with fertility medications to improve success rates, particularly for women over 35 or those with specific fertility challenges. Regular consultations with fertility specialists help determine when additional interventions might be beneficial. We have primarily compared three IUI cycles and one IVF cycle to even up the outcomes. Several well-conducted studies recommend IUI as first-line therapy. Three RCTs compared IUI and IVF. These trials employed ovarian stimulation with IUI and found similar live birth results for 3–6 IUI cycles and 1–2 IVF rounds.
The Cochrane review of treatment-naive women found no difference in live birth rates between IVF and IUI with gonadotropin ovarian stimulation. A sensitivity analysis based on age and previous IUI or IVF treatment showed that there was no significant difference in the live birth rates (RR 1.01, 95% CI 0.88–1.15) among women under 38 who had never had any kind of fertility treatment. Importantly, multiple pregnancy rates were the same.
IUI is cheaper than IVF and requires no specific infrastructure. IUI with ovarian stimulation consistently costs less per live baby than IVF. In an extensive UK research study using the Human Fertilisation and Embryology Authority (HFEA) database, Bahadur and colleagues found that IUI is safer and cheaper per live birth than IVF for unexplained infertility. Couples with unexplained infertility regularly resort to ICSI, a costly and laborious therapy that lacks evidence of improving pregnancy chances.
In countries with limited resources and where IVF is unavailable or costly, IUI is typically the sole treatment for unexplained infertility. In other nations where private IVF facilities prevail, IUI is generally unprofitable compared to IVF.
The IUI procedure can be improved. More strict cancellation criteria for low-dose gonadotropin ovarian stimulation will decrease multiple pregnancies. Using slow-release insemination instead of a bolus may also improve outcomes. A sustained low concentration of spermatozoa may extend potential fertilization, matching physiological processes better than bolus insemination.
For patients, IUI is less intrusive, safer, and more compliant than IVF, which has a high drop-out rate. You cannot use IUI again after IVF. One year after the ‘diagnosis’ of unexplained infertility, the likelihood of natural conceptions is high, and this trend persists for another two years. If treated at these times, it seems more sensible to use IUI, which offers a fair chance of a natural or medically assisted conception, and reserve IVF for those who fail.
When to Seek Further Assistance
After several unsuccessful IUI cycles, couples should discuss alternative treatment options with their healthcare providers. Generally, if pregnancy has not occurred after 3-4 IUI cycles, couples may consider more advanced treatments like IVF. Factors such as age, underlying fertility issues, and previous response to treatment influence this decision.
Conclusion
Success with IUI requires a comprehensive approach combining medical expertise, lifestyle modifications, and emotional support. By understanding the process and implementing appropriate strategies, patients can maximize their chances of achieving pregnancy through IUI. Regular communication with healthcare providers and maintaining realistic expectations help navigate the journey effectively. We strongly recommend visiting Ovum Fertility for the best care and cure of such issues.
FAQs
1.How many IUI cycles should we try before considering other options?
Most fertility specialists recommend trying 3–4 IUI cycles before considering alternative treatments, like IVF. However, this recommendation may vary based on factors such as age, fertility diagnosis, and previous response to treatment. Women over 35 might consider fewer cycles before moving to more aggressive treatments.
2.Does bed rest after IUI improve success rates?
Research shows that extended bed rest after IUI doesn’t significantly improve success rates. You can resume normal activities immediately after the procedure, but we recommend avoiding strenuous exercise for 24-48 hours. The key is maintaining a balanced, stress-free routine during the two-week waiting period.
3.How important is timing for IUI success?
Timing is crucial for IUI success. Perform the procedure within 24-36 hours of ovulation or trigger shot administration. Regular monitoring through ultrasound and blood tests helps determine the optimal timing for each individual cycle.
4.Can lifestyle changes really impact IUI success rates?
Yes, lifestyle modifications can significantly impact IUI success rates. Maintaining a healthy weight, following a balanced diet rich in fertility-supporting nutrients, managing stress levels, and avoiding harmful substances like tobacco and excessive alcohol can improve treatment outcomes.
5.What role does male partner preparation play in IUI success?
Male partner preparation is crucial for IUI success. This includes maintaining excellent overall health, avoiding substances that can affect sperm quality, and following specific instructions regarding abstinence before sperm collection. The quality and quantity of sperm significantly influence IUI outcomes.