Free Fertility Screening
- Fertility Specialist Consultation
- 1st TVS Scan
- Semen Analysis level – 1
65%
IVF success rate
5000+
Trusted Families
10+
Years of Experience
65% IVF success rate
5000+ Trusted Families
10+ Years of Experience
Limited to first 100 customersacross all Ovum Fertility Centres
| Free Fertility Screening | IUI | IVF | Fertility Check up | |
|---|---|---|---|---|
| Cost | Free | ₹6,000 | ₹75,000 | ₹999 |
| Inclusions |
|
|
| |
| Exclusion |
| |||
| *Terms & Conditions Applied | ||||
—
Our Services, The care we provide to our patients 24/7
We offer a full spectrum of reproductive services to address diverse needs:
Your journey to parenthood starts here. With six ART‑registered centres across Bengaluru, Ovum Fertility by Ovum Hospitals offers compassionate, advanced reproductive care in a nurturing environment.
Book an AppointmentYour journey to parenthood starts here. With six ART‑registered centres across Bengaluru, Ovum Fertility by Ovum Hospitals offers compassionate, advanced reproductive care in a nurturing environment.
Laparoscopy is a surgical method for direct visualization of the abdominal cavity. It is an extremely valuable tool in assessing the cause for difficulty in conception.

Embryo transfer is a simple procedure that follows IVF and is often considered the simplest and final step of the IVF process.
Hysteroscopy is the inspection of the uterine cavity that allows diagnosis and treatment of various uterine abnormalities which could lead to fertility problems.
At the heart of your journey
At Ovum, our team delivers care that’s personal, proactive, and truly compassionate.

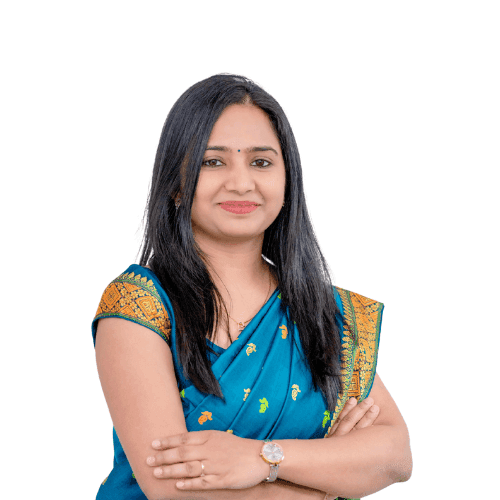
Clinical Director & Lead Consultant - Reproductive Medicine
Kalyan Nagar

Senior Consultant - Reproductive Medicine
Kalyan Nagar
Consultant - Reproductive Medicine
Hoskote

Consultant - Reproductive Medicine
Hennur Road

Consultant - Reproductive Medicine
Bhattarahalli
Our Services, The care we provide to our patients 24/7
We offer round-the-clock support and treatment.
Top fertility specialists, embryologists, and counselors.
65% IVF success rate and 5,000+ families helped.

World-class labs for IVF, ICSI, freezing, and genetic screening.
Compassionate care for your mind and heart.
No hidden costs, just honest care every time.
Treatments tailored to your unique fertility needs.
Sangram Banik
After years of trying to conceive and facing countless disappointments, walking into Ovum Fertility Centre, Bengaluru was like finally seeing light at the end of a very long tunnel. From the first consultation to the final outcome, every step of the journey felt supported, informed, and deeply personal.
Mrs. Geetha S & Manjunatha TV
We are beyond grateful for the exceptional care and support we received throughout our IVF journey. From the very first consultation, the team was compassionate, knowledgeable, and always available to answer our questions. They made a complicated process feel manageable, guiding us with professionalism and kindness every step of the way.
Sanchita Banik
I had a very positive experience with Ovum Fertility Centre ,,Bengaluru. From the very beginning, the staff was warm, professional, and extremely supportive. Every step of the process was explained clearly, and I always felt well-informed and cared for. Doctors were not only experienced but also very compassionate, which made a huge difference during such an emotional journey.
Athira T.K
We were trying to conceive for the past 6 years, we visited a lot of doctors in the past few years and then finally we reached ovum fertility. The Doctor is truly an angel. I'm now pregnant. Her dedication and professionalism is very much appreciated. Doctor is very good in handling patients, and is ready to answer every questions/ concern we have even if that is a very silly question. Doctor is very good in explaining the process before each and every step and is very transparent.
Talking about important issues

Clinical Director & Lead Reproductive Medicine Consultant
MBBS, MS‑OBG, FRM, DRM
Increase success rate in IVF treatment

Fertility Specialist
MBBS MS(OBGY), FRM, DRM
Causes of loose vagina

Fertility Specialist
MBBS, MS OBG, FRM, MRCOG (UK)
Need to know about IVF
Know more about your health
#916, 5th A Cross, Outer Ring Road, HRBR Layout, Kalyan Nagar, Bangalore - 560043
# HIG Extension Road, Swamy Vivekananda Nagar, Hoskote, Karnataka 562114
216/A “Panchajanya” 100 feet Outer Ring Road, 2nd Block,3rd Phase Banashankari, 3rd Stage, Bangalore – 560085
11/B, 25th Cross Rd, 2nd Sector, Garden Layout, Sector 2, HSR Layout, Bengaluru, Karnataka 560102
#32, Old Madras Road, Venkatadri Complex, 2nd Floor, Opposite HDFC Bank, Battarahalli, Bengaluru -560049
#2nd Floor, No 33/4, Hennur Main Road, Kothanur, Bengaluru, Karnataka 560077
Sy. No 171, 2nd Floor Saviraj Complex, Bommenahalli Village, Hobli, Budigere Cross, Bidarahalli, Bengaluru, Karnataka - 560049