Conventional IVF, ICSI, IMSI are unable to detect abnormalities passed on genetically by chromosomes. PGS / PGD are diagnostic procedures used for couples with increased risk of passing a chromosomal abnormality or specific genetic disorder on to their children.
PGS / PGD enables the genetic status of an embryo to be determined prior to embryo transfer which can help in better embryo selection for success and decrease chances of abortions due to genetic abnormalities.
PGS is comprehensive chromosome screening that examines embryos for chromosomal abnormalities. All chromosomes are examined to evaluate any gains or losses of chromosomes.
The information includes
- Chromosomal Duplications: An extra copy of chromosome 21 also known as Downs Syndrome and other such conditions
- Chromosomal Deletions: Missing copies of chromosomes
- Sex-chromosome abnormalities: Duplications and deletions of X & Y chromosomes which can cause many abnormalities
PGS aims at improving pregnancy and live birth rates by screening your embryos for chromosomal abnormalities and only implanting chromosomally normal embryos. PGS is used for testing chromosomal abnormalities only, testing of a specific gene or mutation is performed by PGD.
PGD provides indication whether a specific genetic disease affects an embryo. Families affected by any genetic disease should use this test to reduce the risk of their progeny carrying the genetic disease. PGD helps prevent genetic disease and improves success rates for IVF.
Indications For Pgs/Pgd:
- Advanced maternal age
- Recurrent implantation failure
- Recurrent pregnancy loss
- Known genetic diseases in family
- Couple with genetically abnormal baby
TSteps of PGS / PGD:
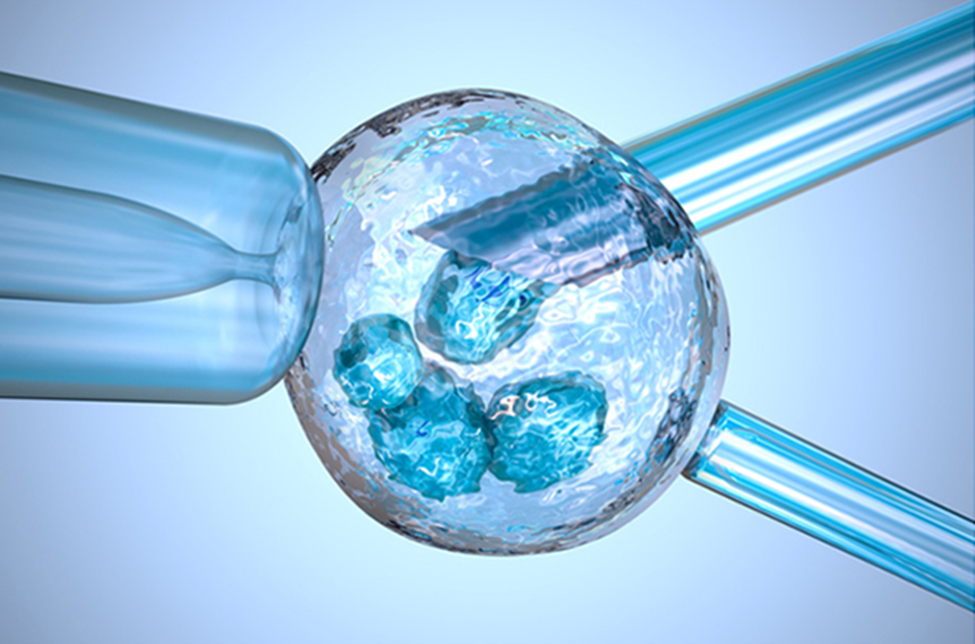
- EEmbryos are formed via In Vitro fertilization (IVF), supplemented by ICSI so as to avoid interference of paternal genes during screening
- Embryos are grown till Day 3 or Day 5
- Embryo biopsy is performed to remove cells from the embryo
- The biopsied cells are processed for PGS or PGD
- Based on the diagnosis, genetically healthy embryos are transferred into the patient
Biopsy for PGS / PGD can be performed on Day 3 embryos (blastomere biopsy) or Day 5 blastocysts (trophectoderm Biopsy). Both day 3 and day 5 biopsy have their own advantages and disadvantages. Various factors need to be considered to decide the day of biopsy.
Day 3 / Blastomere biopsy
On day 3, the embryo comprises of 6- 8 cells & is compactly packed / attached. The Blastomere biopsy removes one of the 8 cells for analysis. As cell size is comparatively large in comparison to day 5 blastocyst cells, it requires a large hole / laser hatching in the embryo shell to remove tightly attached cells. This can be traumatic for an embryo.
Disadvantages: Even though we remove a single cell out of 6-8 cells, the embryo loses a significant part of its total mass. Removal of such a proportionately large percentage of the embryo reduces its developmental potential & subsequently the embryo’s chance of implantation. Also if there is a problem with that one cell only, the results could theoretically, inaccurately represent the rest of the embryo.
Advantages: The results will be available within 48 hrs for the particular embryo & fresh embryo transfer can be performed on day 5.
In this case, the embryo doesn’t need to be frozen while we wait for the results. This will be less expensive since the cost of freezing the embryo and planning frozen embryo transfer is eliminated
Day 5 / Trophectoderm biopsy
On the 5th day, embryos that reached to blastocyst stage comprise of more than 100 cells. Biopsy can be done to remove 8-10 cells at this stage which gives much more accurate results of DNA analysis.
Comparatively smaller portion of the embryo is removed from the outer layer of the embryo destined to form the placenta, called the trophectoderm (TE). The cells that form the baby are undisturbed, preserving the embryo’s true potential & thus less traumatic for an embryo.
In this case, the embryo has to be frozen till the results are obtained and transferred in a subsequent HRT cycle.